Esophagus Diseases
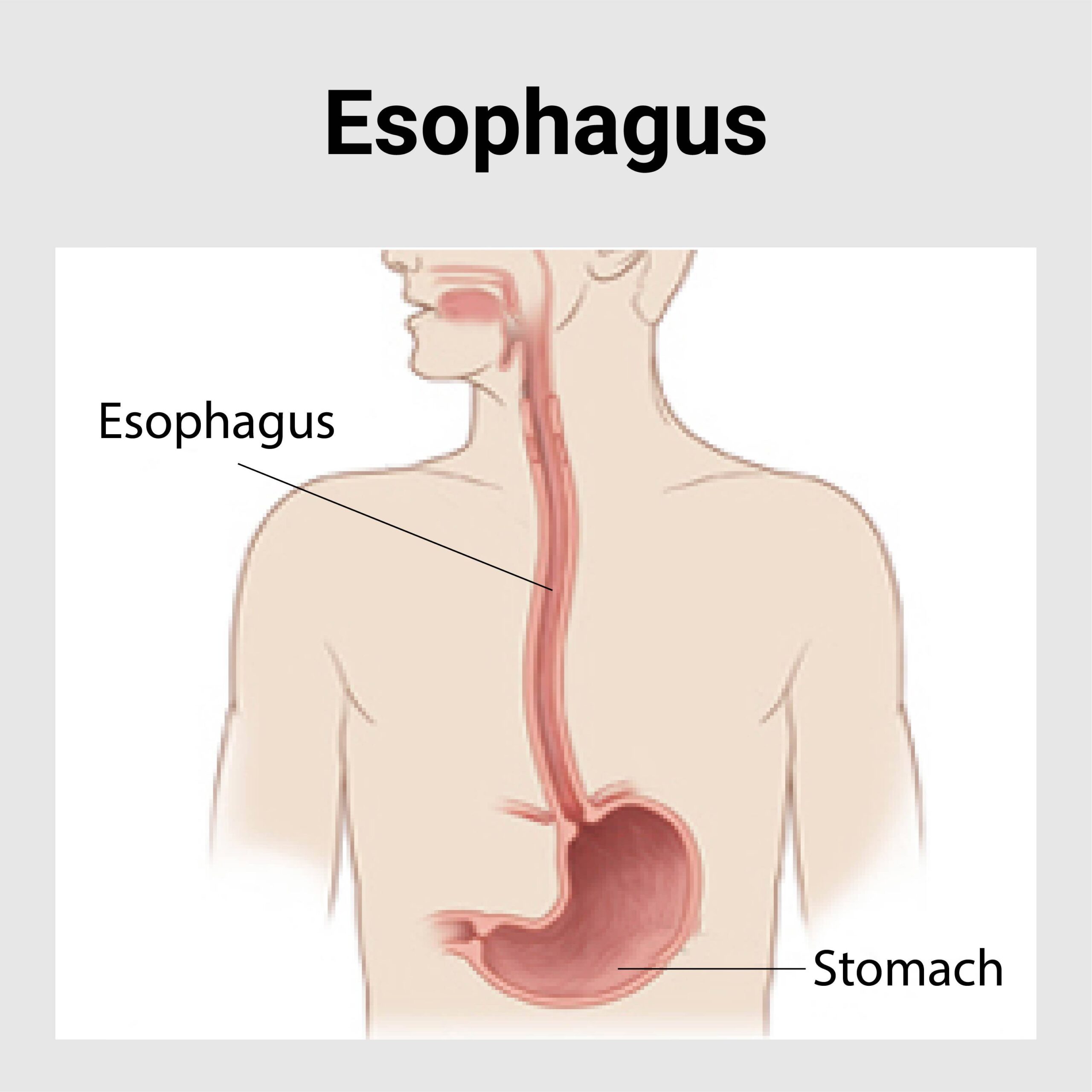
Esophagus is a hollow tube-like muscular structure connecting mouth to the stomach and mainly resides in the neck and chest part of the body. It passes food from the mouth to the stomach.
Diseases of esophagus causes difficulty in deglutition, difficult swallowing as well retrosternal pain or heaviness.
- Gastro Esophageal Reflux Disease (GERD)
- Achalasia Cardia
- Diverticulum of Esophagus
- Foreign Body in Esophagus
- Corrosive Injury of Esophagus
- Cancer of Esophagus
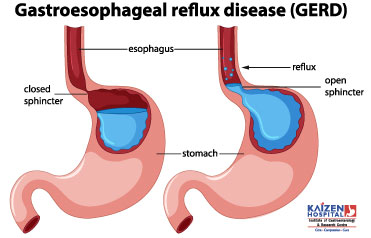
GERD
What are the symptoms of GERD?
- Heartburn: this is the most common symptom. This is a burning feeling which rises from the upper abdomen or lower chest up towards the neck.
- Pain abdomen or chest pain, dyspepsia
- Some uncommon symptoms: these may occur and can make the diagnosis difficult.
- Recurrent cough
- Asthma
- Wheeze
- Sore throat
- Hoarseness of voice
- Tooth and gum problem
- Severe chest pain
What investigations required?
Tests are not usually necessary if you have typical symptoms. You need to have upper GI endoscopy to confirm and establish the extent of damage. There are GERD where endoscopy may be negative. There are other investigations; like 24 hour pH analysis which is highly sensitive test to confirm GERD. Other tests like manometry, chest x ray, ECG might be needed.
What can we do to reduce the symptoms?
The following lifestyle changes may help to reduce the reflux:
- Stop smoking
- Some foods and drinks – Foods and drinks those might be responsible for reflux are peppermints, chocolate, spicy foods, hot drinks, coffee, and alcoholic drinks. Also, avoiding large-volume meals may help. Certain medications like pain killers may worsen the symptoms
- Weight loss – If you are overweight, losing some weight may help to improve the symptoms.
- Posture – Lying down or bending forward may increase reflux. Wearing tight belts may increase intraabdominal pressure and increases the reflux.
- Bedtime
- Avoid sleeping within 2 – 3 hours of meal.
- Raise head end of the bed by 1- 20 cm.
What are the treatment options for GERD?
- Medications – antacids, H2 blockers, proton pump inhibitors, prokinetic agents
- Surgical treatment – laparoscopic fundoplication
- Choice of treatment depends on severity and duration of symptoms, presence or absence of complications.
Are there any complications from GERD?
- Scarring and stricture of esophagus, lung, gum and tooth problem, Barrett\’s esophagus and sometimes cancer of the esophagus.
Achalasia Cardia
Treatment includes medical drug therapy, endoscopic therapy (Pneumatic dilatation or POEM) or surgery cardiomyotomy. Surgery of achalasia cardia known as laparoscopic cardiomyotomy, in which stenosed part of the esophagus muscles are opened up to allow the food smoothly into the stomach. Laparoscopic surgery has added advantage of less pain and reduced hospital stay.
Achalasia Cardia
When we eat the food it passes through the esophagus (food pipe) to the stomach. There is a valve (sphincter) between the esophagus and stomach, which relaxes when food passes from esophagus to stomach. If the sphincter fails to relax; it causes dysphagia (difficulty in swallowing).
What is achalasia cardia?
Achalasia cardia is a motility disease of the esophagus where the sphincter between esophagus and stomach fail to relax and do not allow food to pass easily from esophagus to stomach.
What are the symptoms?
Dysphagia means difficulty in swallowing is the main symptom. Other symptoms can be regurgitation, cough, heart burn, chest pain, weight loss.
What investigation are required?
Chest x ray, endoscopy, barium study are commonly required investigations. Esophageal manometry required to confirm the diagnosis as well as to know the type of achalasia.
What is the treatment?
There are two options for the treatment; surgical treatment and endoscopic treatment. Surgical treatment is the best one-time long-term option. Surgical treatment is laparoscopic cardiomyotomy which is very safe procedure. Endoscopic treatment (Pneumatic dilatation or POEM) is pneumatic dilatation of the sphincter.
Diverticulum of Esophagus
Classification
Esophageal diverticula are classified by their location within the esophagus:
- Zenker’s diverticula (pharyngo-esophageal)-located in the back of the throat, just above the esophagus
- Midthoracic diverticula, in the mid-chest
- Epiphrenic diverticula, above the diaphragm
Symptoms
- Dysphagia
- Regurgitation
- Aspiration pneumonia
- Pulmonary Aspiration
- Cough
- Weight loss
- Neck pain
- Halitosis
Causes
- Internal pressure exerted by the esophagus to propel food into the stomach can herniate the esophageal lining through a weakened wall, creating a pouch or a diverticulum.
- Motility disorders of esophagus like achalasia cardia.
Investigations
- Barium swallow
- UGI Endoscopy
- esophageal manometry
Treatment
- Lifestyle changes such as eating a bland diet, chewing food thoroughly, and drinking plenty of water after meals.
- In case of severe symptoms, surgery may be required to repair the defect.
- If symptoms become severe, several types of surgery are available to remove the diverticula, repair the defects and relieve a patient’s symptoms and improve their quality of life.
Foreign Body in Esophagus
Symptoms
- Gagging, vomiting
- Neck or throat pain
Causes
- Children- Food boluses and accidental swallowing of objects such as coins or marbles.
- Adults- Accidental swallowing of dentures and toothpicks.
Investigations
- Chest PA
- X Ray Abdomen Erect
- CT Scan
- Barium or Gastrografin Swallow
- Ultrasonography
- Endoscopy
Management
- Removal of foreign body by endoscopic or surgical methods.
- Esophageal Foreign Body Complications
Corrosive Injury of Esophagus
Symptoms
- Dysphagia, Odynophagia
- Dyspnoea, Respiratory distress, tachypnoea, hyperpnoea
- Abdominal pain
- Chest pain
- Nausea, Vomiting
Signs
- Cough
- Dysphonia or aphonia
- Hoarseness
- Stridor
- Tachycardia
- Oropharyngeal burns
- Haemetemesis
- Acute peritonitis – Abdominal guarding, rebound tenderness, and diminished bowel sounds
- Altered mental status
- Hypotension
Investigations
- CBC, BUN, Creatinine, Electrolytes, LFT, ABG levels.
- Chest PA to rule out mediastinitis, pleural effusions, aspiration pneumonitis.
- X Ray Abdomen Erect to rule out pneumoperitoneum or ascites.
- Computed tomography (CT) scan
- Upper GI Endoscopy
Emergency Care
Prompt evaluation of airway and vital signs with immediate cardiac monitoring and intravenous access. Intravenous fluids and blood products may be required in case of excessive bleeding or vomiting. Needs hospitalization and sometime endoscopic examination of upper GI tract and upper respiratory tract.
Complications
- Airway oedema or obstruction
- Mediastinitis, pericarditis, pleuritis, esophageal-aortic fistula formation, tracheoesophageal fistula formation, peritonitis.
- Gastroesophageal perforation, Haemorrhage
- Gastric outlet obstruction
- Cardiac arrest
Long-term risks include squamous cell carcinoma, which occurs in 1-4% of all significant exposures and may occur as late as 40 years after exposure.
Cancer of Esophagus
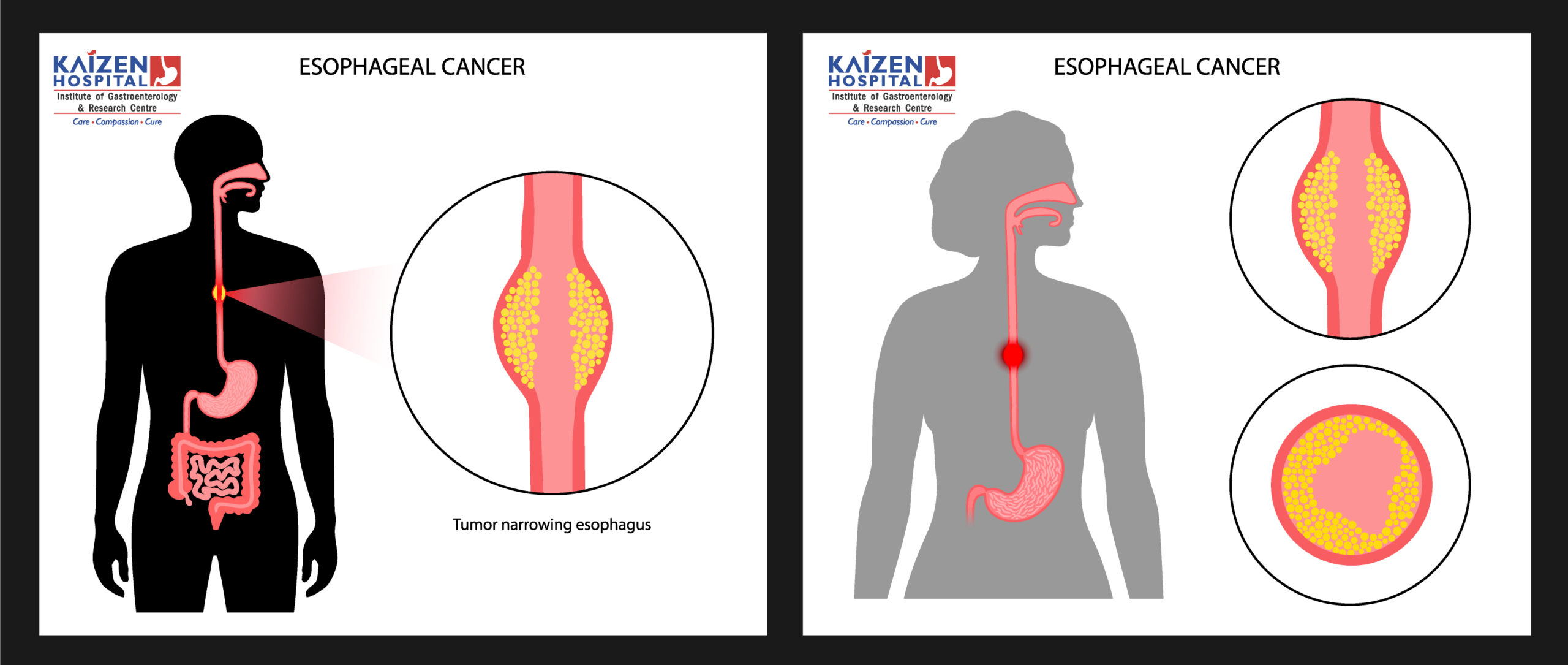
The two main sub-types of esophageal cancer are squamous cell carcinoma, which is more common in the developing world, and adenocarcinoma, which is more common in the developed world. A number of less common types also occur. Squamous-cell carcinoma arises from the skin cells that line the esophagus. Adenocarcinoma arises from glandular cells present in the lower third of the esophagus, often where they have already transformed to intestinal cell type (a condition known as Barrett’s esophagus). The most common causes of the squamous-cell type are tobacco, alcohol, very hot drinks, and a poor diet. The most common causes of the adenocarcinoma type are smoking tobacco, obesity, and acid reflux.
The disease is diagnosed by a biopsy done by an endoscope (a fiber optic camera). Prevention includes stopping smoking and a healthy diet. Treatment is based on cancer’s stage and location, together with the person’s general condition and individual preferences. Small localized squamous-cell cancers may be treated with surgery alone with the hope of a cure. In most other cases, chemotherapy with or without radiation therapy is used along with surgery. Larger tumors may have their growth slowed with chemotherapy and radiation therapy. In the presence of extensive disease or if the affected person is not fit enough to undergo surgery, palliative care is often recommended. Outcomes are related to the extent of the disease and other medical conditions but generally tend to be fairly poor, as the diagnosis is often late. Five-year survival rates are around 13% to 18%.
Signs and symptoms
Prominent symptoms usually do not appear until cancer has infiltrated over 60% of the tube’s circumference, by which time the tumor is already in an advanced stage. The onset of symptoms is usually caused by narrowing of the tube due to the physical presence of the tumor.
The first and the most common symptom is usually difficulty in swallowing, often initially experienced with solid foods and later with softer foods and liquids. Pain when swallowing is less usual initially. Weight loss is often an initial symptom in cases of squamous-cell carcinoma, though not usually in cases of adenocarcinoma. Eventual weight loss due to reduced appetite and undernutrition is common. Pain behind the breastbone or in the region around the stomach often feels like heartburn. The pain can frequently be severe, worsening when food of any sort is swallowed. Another sign may be an unusually husky, raspy, or a hoarse-sounding cough, a result of the tumor affecting the recurrent laryngeal nerve.
The presence of the tumor may disrupt the normal contractions of the esophagus on swallowing. This can lead to nausea and vomiting, regurgitation of food, coughing, and an increased risk of aspiration pneumonia. Abnormal connections (fistulas) occasionally develop between the esophagus and the trachea (windpipe). Early signs of this serious complication may be coughing on drinking or eating. Fistulas often lead to pneumonia, typical signs of which are a cough, fever, or aspiration. The tumor surface may be fragile and bleed, causing vomiting of blood. Compression of local structures occurs in advanced disease, leading to such problems as upper airway obstruction and superior vena cava syndrome.
If cancer has spread elsewhere, symptoms related to metastatic disease may appear. Common sites of spread include nearby lymph nodes, the liver, lungs, and bone. Liver metastasis can cause jaundice and abdominal swelling (ascites). Lung metastasis can cause, among other symptoms, impaired breathing due to excess fluid around the lungs (pleural effusion), and dyspnea (the feelings often associated with impaired breathing).
Causes
The two main types (i.e. squamous-cell carcinoma and adenocarcinoma) have distinct sets of risk factors. Squamous-cell carcinoma is linked to lifestyle factors such as smoking and alcohol. Adenocarcinoma has been linked to effects of long-term acid reflux. Tobacco is a risk factor for both types. Both types are more common in men and in the over-60s.
Squamous-cell carcinoma
The two major risk factors for esophageal squamous-cell carcinoma are tobacco (smoking or chewing) and alcohol. The combination of tobacco and alcohol has a strong synergistic effect. Some data suggest that about half of all cases are due to tobacco and about one-third to alcohol, while over three-quarters of the cases in men are due to the combination of smoking and heavy drinking. The risks associated with alcohol appear to be linked to its aldehyde metabolite and to mutations in certain related enzymes.
High levels of dietary exposure to nitrosamines (chemical compounds found both in tobacco smoke and certain foodstuffs) appear to be a relevant risk factor. Unfavorable dietary patterns seem to involve exposure to nitrosamines through processed and barbecued meats, pickled vegetables, etc., and a low intake of fresh foods. Other associated factors include nutritional deficiencies, low socioeconomic status, and poor oral hygiene. Chewing betel nut (areca) is an important risk factor in Asia.
Adenocarcinoma
Male predominance is particularly strong in this type of esophageal cancer, which occurs about 7 to 10 times more frequently in men. This imbalance may be related to the characteristics and interactions of other known risk factors, including acid reflux and obesity.
The long-term erosive effects of acid reflux (an extremely common condition, also known as gastroesophageal reflux disease or GERD) have been strongly linked to this type of cancer. Longstanding GERD can induce a change of cell type in the lower portion of the esophagus in response to the erosion of its squamous lining. This phenomenon, known as Barrett’s esophagus, seems to appear about 20 years later in women than in men, maybe due to hormonal factors. Having symptomatic GERD or bile reflux makes Barrett’s esophagus more likely, which in turn raises the risk of further changes that can ultimately lead to adenocarcinoma. The risk of developing adenocarcinoma in the presence of Barrett’s esophagus is unclear, and may in the past have been overestimated.
Obesity and overweight both appear to be associated with increased risk. The association with obesity seems to be the strongest of any type of obesity-related cancer, though the reasons for this remain unclear. Abdominal obesity seems to be of particular relevance, given the closeness of its association with this type of cancer, as well as with both GERD and Barrett’s esophagus. This type of obesity is characteristic of men. Physiologically, it stimulates GERD and also has other chronic inflammatory effects.
Diagnosis
Clinical evaluation
Although an occlusive tumor may be suspected on a barium swallow or barium meal, the diagnosis is best made with esophagogastroduodenoscopy (endoscopy) this involves the passing of a flexible tube with a light and camera down the esophagus and examining the wall. Biopsies taken of suspicious lesions are then examined histologically for signs of malignancy.
Additional testing is usually performed to estimate the tumor stage, for which the TNM staging system is used. Computed tomography (CT) of the chest, abdomen, and pelvis can evaluate whether cancer has spread to adjacent tissues or distant organs (especially liver and lymph nodes). The sensitivity of a CT scan is limited by its ability to detect masses (e.g. enlarged lymph nodes or involved organs) generally larger than 1 cm. Positron emission tomography is also used to estimate the extent of the disease and is regarded as more precise than CT alone. Esophageal endoscopic ultrasound can provide staging information regarding the level of tumor invasion, and possible spread to regional lymph nodes.
The location of the tumor is generally measured by the distance from the teeth. The esophagus (25 cm or 10 in long) is commonly divided into three parts for purposes of determining the location. Adenocarcinomas tend to occur nearer the stomach and squamous cell carcinomas nearer the throat, but either may arise anywhere in the esophagus.
Classification
Esophageal cancers are typically carcinomas which arise from the epithelium, or surface lining, of the esophagus. Most esophageal cancers fall into one of two classes: squamous-cell carcinomas, which are similar to head and neck cancer in their appearance and association with tobacco and alcohol consumption, and adenocarcinomas, which are often associated with a history of GERD and Barrett’s esophagus. A general rule of thumb is that a cancer in the upper two-thirds is likely to be a squamous-cell carcinoma and one in the lower one-third an adenocarcinoma. Rare histologic types of esophageal cancer are different variants of the squamous-cell carcinoma, and nonepithelial tumors, such as leiomyosarcoma, malignant melanoma, rhabdomyosarcoma, lymphoma, and others.
Prevention
Prevention includes stopping smoking or chewing tobacco. Overcoming addiction to areca chewing in Asia is another promising strategy for the prevention of esophageal squamous-cell carcinoma.
According to the National Cancer Institute, “diets high in cruciferous (cabbage, broccoli, cauliflower, Brussels sprouts) and green and yellow vegetables and fruits are associated with a decreased risk of esophageal cancer” Dietary fiber is thought to be protective, especially against esophageal adenocarcinoma.
Screening
People with Barrett esophagus (a change in the cells lining the lower esophagus) are at much higher risk and may receive regular endoscopic screening for the early signs of cancer. Because the benefit of screening for adenocarcinoma in people without symptoms is unclear, it is not recommended in the United States. Some areas of the world with high rates of squamous-carcinoma have screening programs.
Management
The treatment is determined by the cellular type of cancer (adenocarcinoma or squamous-cell carcinoma vs other types), the stage of the disease, the general condition of the patient, and other diseases present. Treatment should be managed by a multidisciplinary team covering the various specialities involved. Adequate nutrition needs to be assured, and adequate dental care is vital.
A number of types and combinations of surgery, chemotherapy, and radiotherapy, as well as other therapies, have been used over recent decades, but there has been no transformative improvement in outlook for patients equivalent to that seen in some other cancers.
Surgery
Early-stage adenocarcinomas will be treated by surgery where this is possible, although esophagectomy, the removal of all or part of the esophagus, is a difficult operation with a relatively high risk of mortality or post-operative difficulties; the benefits of surgery are less clear for early-stage squamous cancers. There are a number of surgical options, and the best choices for particular situations remain the subject of research and discussion. As well as the characteristics and location of the tumor, other factors include the condition of the patient and the type of operation to which the surgical team is most used. Surgical outcomes are likely to be better in large centers where the procedures are frequently performed. If cancer has spread to other parts of the body, esophagectomy will now not normally be performed.
Endoscopic mucosal resection (EMR) is the removal of small tumors that only involve the mucosa or lining of the esophagus (stage T1a).
Esophagectomy is the removal of a segment of the esophagus; as this shortens the length of the remaining esophagus, some other segment of the digestive tract is pulled up through the chest cavity and interposed. This is usually the stomach or part of the large intestine (colon) or the jejunum. The joining up of the stomach to a shortened esophagus is called an esophagogastric anastomosis.
There are a number of different methods of esophagectomy; which is used will depend on the nature and location of the tumor, and the preference of the surgeon. Clear evidence from clinical trials for which approaches give the best outcomes in different circumstances is lacking. The first distinction, based on how the surgeon enters the body, is between transcranial procedures as opposed to a transthoracic. The more recent transhiatial approach avoids the need to open the chest; instead, the surgeon enters the body through an incision in the lower abdomen and another in the neck. The esophagus is freed from the surrounding tissues and cut away as necessary. The stomach is then pushed through the esophageal hiatus, the hole in the diaphragm of the esophagus, and joined to the remaining upper part of the esophagus at the neck.
The traditional transthoracic approach enters the body through the chest, and has a number of variations: the thoraco abdominal approach opens the abdominal and thoracic cavities together, the two-stage Ivor Lewis (also called Lewis Tanner) approach involves an initial laparotomy and construction of a gastric tube, followed by a right thoracotomy to excise the tumor and create an esophagogastric anastomosis, the three-stage McKeown approach adds a third incision in the neck to complete the cervical anastomosis. Recent approaches by some surgeons use what is called extended esophagectomy, where more surrounding tissue including lymph nodes is removed en bloc.
If the person cannot swallow at all, an esophageal stent may be inserted to keep the esophagus open; stents may also assist in occluding fistulas. A nasogastric tube may be necessary to continue feeding while treatment for the tumor is given, and some patients require a gastrostomy (feeding hole in the skin that gives direct access to the stomach). The latter two are especially important if the patient tends to aspirate food or saliva into the airways, predisposing
for aspiration pneumonia.
Chemotherapy and radiotherapy
Chemotherapy depends on the tumor type but tends to be cisplatin-based (or carboplatin or oxaliplatin) every three weeks with fluorouracil (5-FU) either continuously or every three weeks. In more recent studies, the addition of epirubicin was better than other comparable regimens in advanced non resectable cancer. Chemotherapy may be given after surgery (adjuvant, i.e. to reduce the risk of recurrence), before surgery (neoadjuvant) or if surgery is not possible; in this case, cisplatin and 5-FU are used. Ongoing trials compare various combinations of chemotherapy; the phase II/III REAL-2 trial, for example, compares four regimens containing epirubicin and either cisplatin or oxaliplatin, and either continuously infused fluorouracil or capecitabine.
Radiotherapy is given before, during, or after chemotherapy or surgery, and sometimes on its own to control symptoms. In patients with localized disease but contraindications to surgery, “radical radiotherapy” may be used with curative intent.
Prognosis
In general, the prognosis of esophageal cancer is quite poor, because most patients present with advanced disease. By the time the first symptoms (such as difficulty swallowing) appear, cancer has already well progressed. The overall five-year survival rate (5YSR) in the United States is around 15%, with most people dying within the first year of diagnosis.
Individualized prognosis depends largely on stage. Those with cancer restricted entirely to the esophageal mucosa have about an 80% 5YSR, but submucosal involvement brings this down to less than 50%. Extension into the muscularis propria (muscle layer of the esophagus) suggests a 20% 5YSR, an extension to the structures adjacent to the esophagus predict a 7% 5YSR. Patients with distant metastases (who are not candidates for curative surgery) have a less than 3% 5YSR.
HOSPITAL ADDRESS
132ft. Ring Road, Helmet Circle, Memnagar, Ahmedabad – 380052. Gujarat, India.
EMERGENCY( 24X7 )
Mobile: +91 – 99047 44410
Help Line : +91 – 98244 40044
+91 – 79 – 2791 4444
E-MAIL ADDRESS
contact@xdemo.app
WHY KAIZEN ?
With a vision to extend World Class healthcare solutions to the community through advances in medical technology, medical research and by adopting best man power management practices , Kaizen hospital was established in Ahmedabad in 2011.

