Liver Disease
The liver is a vital organ of vertebrates and some other animals.In the human, it is located in the upper right quadrant of the abdomen, below the diaphragm. The liver has a wide range of functions, including detoxification of various metabolites, protein synthesis, and the production of biochemicals necessary for digestion.
The liver is a gland and plays a major role in metabolism with numerous functions in the human body, including regulation of glycogen storage, decomposition of red blood cells, plasma protein synthesis hormone production, and detoxification.
Common Diseases of Liver are :
- Cirrhosis of Liver
- Portal Hypertension
- Hydatid Cyst of Liver
- Liver Injury
- Liver Abscess
- Cancer of Liver
Cirrhosis of Liver
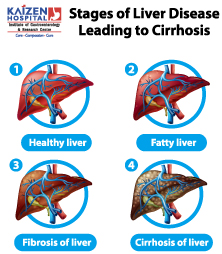
Causes
- Chronic alcohol abuse
- Fat accumulating in the liver (non alcoholic fatty liver disease)
- Hepatitis B and C
- Iron build up in the body (haemochromatosis)
- Inherited disorders of sugar metabolism (galactosemia or glycogen storage disease)
- Autoimmune hepatitis
- Genetic digestive disorder (Alagille syndrome)
- Cystic fibrosis
- Primary biliary cirrhosis
- Accumulation of Copper in the liver (Wilson’s disease)
- Hardening and scarring of the bile ducts (primary sclerosing cholangitis)
- Poorly formed bile ducts (biliary atresia)
- Infection by a parasite common in developing countries (schistosomiasis)
Symptoms
- Fatigue
- Anorexia
- Cachexia
- Pedal oedema
- Pruritus
- Confusion, drowsiness and slurred speech (Hepatic Encephalopathy)
- Spider naevi
- Nausea
- Yellowish discoloration in the skin,eyes and urine (Jaundice)
- Ascites
- Easy tendency to bleed and bruise
Diagnosis
- LFT, RFT
- Viral Hepatitis markers
- PT INR
- USG Abdomen
- CT Scan
- MRE (Magnetic Resonance Elastography)
- UGI scopy with biopsy
Treatments and drugs
- Avoid drinking alcohol.
- Lose weight.
- Medical treatment
- Surgery- Liver transplant
Complications
- Portal Hypertension
- Jaundice
- Stones in Gall Bladder and Bile Ducts
- Ascites
- Pedal oedema
- Oesophageal or Gastric Varices which can lead to bleeding
- Splenomegaly
- Infections
- Malnutrition
- Hepatic Encephalopathy
- Bone disease
- Liver Cancer
Portal Hypertension
- Prehepatic – Portal vein thrombosis or congenital atresia.
- Intra hepatic – liver cirrhosis, hepatic fibrosis, non cirrhotic causes and diffuse granulomatous diseases
- Post hepatic – Hepatic vein thrombosis, inferior vena cava thrombosis, inferior vena cava congenital malformation, and constrictive pericarditis.
Signs and symptoms
- Ascites
- Splenomegaly
- Hepatic encephalopathy.
- Esophageal, gastric and ano rectal varices
- Haemetemsis
- Malaena
- Bacterial Peritonitis
Diagnosis
- HVPG (hepatic venous pressure gradient)
- Contrast Angiography
Treatment
- Porto systemic shunts
- Prevention of bleeding
- Endoscopic banding ligation in case of varices.
- Diuretics, paracentesis in case of ascites
Hydatid Cyst of Liver
Etiology
- Echinococcosis is caused by larval cestodes of the phylum Platyhelminthes (tapeworms).
- Hydatid disease in humans is caused by contact with dog feces or dog hair infected with the tapeworm eggs, or contaminated vegetables. Hydatid disease is not contagious and is not passed by person-to-person contact.
Symptoms
- The symptoms of hydatid disease vary according to body organs which are infected. The most commonly infected organs are the liver, lungs, muscles, bones, kidneys, brain, and spleen.
- Symptoms can occur a long time after infection and sometimes many years later, but there may be no symptoms at all. Symptoms may include:
- Weight loss
- Abdominal distention
- Biliary colic
- Jaundice
- Urticaria
- Anaemia
- Fatigue
- Chronic cough
- Dyspnoea
- Chest pain
- Hemoptysis
- Headache, dizziness
- Malnutrition
Diagnosis
- Thorough medical history and physical examination
- Chest X-ray
- Ultrasound
- CT Scan
- MRI
- Examination of blood, urine, sputum and feces
- Blood tests for antibodies to the cysts
Treatment
- Surgery combined with drugs such as albendazole and/or mebendazole before surgery and for 8 weeks after surgery to clear up tapeworm infection.
- In case of cysts in multiple organs or tissues, drugs (Albendazole or Mebendazole) and/or PAIR (puncture-aspiration-injection-reaspiration) become the only possible treatment.
- There is a new treatment called Percutaneous Thermal Ablation (PTA) of the germinal layer in the cyst by radiofrequency ablation device.
Complications
- Recurrence
- Infection
- A rupture into the biliary tree can lead to obstruction by the daughter cysts, producing cholangitis.
- Metastasis
- Rupture into the bronchi can lead to expectoration of cyst fluid.
- Cystobiliary fistula
- Spillage and seeding
- Allergic reaction or anaphylactic shock
Liver Injury
- Blunt abdominal trauma caused by vehicular accident
- Penetrating trauma caused by knife or gunshot injury
Symptoms
- Abdominal pain
- Haemorrhage
- Tachycardia
- Tachypnoea
Diagnosis
- Ultrasound
- CT Scan
Treatment
- Hospitalisation
- Blood Transfusion in case of massive bleeding
- Surgery
Liver Abscess
A liver abscess is pus-filled mass inside the liver.
Types
- Pyogenic liver abscess
- Amoebic liver abscess
- Fungal abscess
Causes
- Bacterial infection
- Ruptured appendix
- Colon cancer
- Pancreatic Cancer
- IBD
- Septicaemia
- Trauma to Liver
Symptoms
- Fever with rigors
- Right upper abdominal pain
- Weight loss
- Vomiting, diarrhoea
- Dark coloured urine
- Whitish or clay-coloured stool
Diagnosis
- CBC
- Blood Culture
- USG Abdomen
- CT Scan
Treatment
- Drainage of abscess
- CT guided biopsy
Complications
- Sepsis
Cancer of Liver
Primary liver cancer means that the cancer started (originated) in the liver. In the UK, primary liver cancer is uncommon. There are around 3,000 cases of primary liver cancer each year in the UK. It occurs most commonly in people aged over 65 years. However, worldwide, it is one of the most common cancers.
Secondary (metastatic) liver cancer means that a cancer which started in another part of the body has spread to the liver. Many types of cancer can spread to the liver. Most commonly, cancers of the bowel, pancreas, stomach, lung or breast. The
behavior, treatment and outlook of secondary liver cancers are often quite different to primary liver cancer.
There are different types of primary liver cancer which include:
- Hepatoma: This is the most common type (about 9 in 10 cases). It is sometimes called hepatocellular carcinoma (HCC). This type of cancer originates from a liver cell (hepatocyte) which becomes cancerous. (The bulk of the liver is made up from hepatocytes). A hepatoma most commonly develops as a complication of liver diseases such as cirrhosis (scarring of the liver) or types of hepatitis (liver inflammation).
- Fibrolamellar hepatoma is a rare subtype of hepatoma. It typically develops in a liver which was previously healthy.
- Cholangiocarcinoma: This is uncommon. It develops from cells which line the bile duct.
- Hepatoblastoma: This is a rare cancer which occurs in some young children.
- Angiosarcoma: This is rare. It develops from blood vessel cells within the liver.
What causes liver cancer?
A cancerous tumor starts from one abnormal cell. The exact reason why a cell becomes cancerous is unclear. It is thought that something damages or alters certain genes in the cell. These make the cell abnormal and multiply out of control.
Most people who develop a primary liver cancer have one or more of the following risk factors which seem to make liver cells more prone to becoming cancerous:
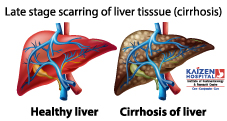
- Cirrhosis. This is a condition which causes scarring of the liver. It tends to progress slowly. In the UK, the common causes of cirrhosis are heavy alcohol drinking, and infection with hepatitis C. However, there are various other causes of
cirrhosis. Note: most people with cirrhosis do not develop liver cancer – it occurs in only a small number of people with cirrhosis. - Long-term infection with the hepatitis B or hepatitis C virus. It typically takes 20-30 years after first becoming infected to develop primary liver cancer. Infection with these viruses is not common in the UK, but it is becoming more common. However, these are common infections worldwide, particularly in Asia and Africa. Many young children in these areas are infected with the hepatitis B virus. This is why primary liver cancer is a common cancer in young adults in these areas of the world (developing 20-30 years after first being infected).
- Ingesting some poisons or toxins. For example, a known risk factor is a poison called aflatoxin which contaminates some foods (for example, mouldy peanuts), mainly in developing countries.
- Some conditions which cause persistent inflammation of the gut increase the risk slightly of developing a cholangiocarcinoma (an uncommon type of primary liver cancer) – for example, ulcerative colitis.
- There is some evidence that smoking can increase the risk
- A parasitic infection (liver fluke) which mainly occurs in Africa and Asia increases the risk of developing a cholangiocarcinoma.
What are the symptoms of liver cancer?
There may be no symptoms in the early stage of the disease. As the cancer grows, the first symptoms to develop may be quite vague and nonspecific. For example, feeling generally unwell, feeling sick (nausea), loss of appetite, weight loss and tiredness. Many people who develop primary liver cancer will already have symptoms associated with cirrhosis. If you already have cirrhosis and your health becomes worse quite quickly, the cause may be a liver cancer which has developed.
As the cancer develops further, more specific symptoms which may also develop include:
- Abdominal pain over the liver area.
- Jaundice. Jaundice is when you go yellow. You tend to first notice it when the whites of the eyes become yellow. It is due to a build-up of the chemical bilirubin which is made in the liver. This occurs if the bile duct becomes blocked by the
cancer. Bile and bilirubin cannot drain out from the liver and so leak into the bloodstream. - Itch (caused by the jaundice).
- Swelling of the abdomen. This can be due to the growing cancer itself. It may also be due to ascites which is fluid that builds up in the abdomen which occurs with various liver disorders.
How is cancer of the liver diagnosed and assessed?
Screening
Screening using ultrasound, and sometimes also a blood test for alpha-fetoprotein (AFP), at 6- to 12-month intervals, has been recommended for people at high risk of liver cancer. This includes people with liver cirrhosis associated with infection with hepatitis B or hepatitis C virus. This can detect liver cancer at an earlier stage and therefore improve the chance of successful treatment.
Initial assessment
If liver cancer is suspected, you are likely to have a number of tests. These aim to:
- Confirm that you have a cancer in the liver. Also, that the cancer is a primary liver cancer and not a secondary liver cancer.
- Assess the stage of the cancer. That is, how much of the liver is affected and whether the cancer has spread to other parts of the body.
- Assess the state of your liver function and your general health.
- Therefore, a range of tests are usually needed. They may include:
- Scans such as ultrasound scan, CT scan or MRI scan. These can help to show the exact location and extent of the cancer.
- A liver biopsy. This is usually done to confirm the type of cancer. A biopsy is when a small sample of tissue is removed from a part of the body.
- The sample is then examined under the microscope to look for abnormal cells.
- Blood tests help to assess the liver function and your general health.
- Other tests may be done if the above do not clarify the situation. For example, a laparoscopy is sometimes done. This is a small operation to look inside the abdomen with a flexible telescope.
What are the treatment options for liver cancer?
The main treatments used for liver cancer are surgery and chemotherapy. Other techniques are sometimes used. The treatment advised in each case depends on various factors such as:
- The exact site of the primary tumour in the liver.
- The stage of the cancer (how large the cancer is and whether it has spread). See also separate leaflet called Staging and grading cancer.
- Your general health. In particular, the general state of your liver and liver function (many people with primary liver cancer also have poor liver function due to cirrhosis).
Surgery
Surgery which aims to cure the cancer is an option in some cases. If the cancer is small, has not spread outside the liver, and the rest of the liver is healthy, then it may be possible to cut out the part of the liver which contains the cancer. Healthy liver tissue will regrow to its full size within a few weeks if a section of liver is cut out. However, this operation is not suitable if your liver is damaged with severe cirrhosis (which is the case in many people with primary liver cancer). A liver transplant is another option, but again only suitable for a small number of cases.
Surgery also has a role in palliative care. For example, if jaundice is severe, it may be possible to relieve the blockage of the bile by inserting a stent.
This is a narrow tube which allows the bile to drain into the gut. Another example is to ease ascites (fluid in the abdomen) if it is severe. The ascites can be drained by inserting a tube through the wall of the abdomen.
Chemotherapy
Chemotherapy is a treatment which uses anti-cancer medicines to kill cancer cells, or to stop them from multiplying. It is not likely to be curative for primary liver cancer, but may shrink the tumour down to slow the progression of the disease.
There are new medicines being developed for the treatment of liver cancer. For example, sorafenib is a type of medicine called a multi-targeted kinase inhibitor. It interferes with the growth of cancer cells. Research has shown that sorafenib can be beneficial for people with advanced hepatocellular carcinoma. However, sorafenib is not currently recommended by the National Institute for Health and Clinical Excellence (NICE) for the treatment of people with advanced hepatocellular carcinoma.
Other treatments
Various other treatment techniques are sometimes used. For example:
- Alcohol ablation. Ablation means to destroy. For this treatment, alcohol is injected into the tumour. The alcohol kills cancer cells.
- Radiofrequency ablation. For this treatment, a needle is inserted into the tumour. High-intensity radio waves or laser light are then passed hrough the needle. This heats the cancer cells and kills them.
- Cryotherapy. For this treatment, a small metal object filled with liquid nitrogen is placed into the tumour. The liquid nitrogen makes it very cold which destroys cancer cells.
- Chemoembolisation. For this treatment, medicines used for chemotherapy are mixed with another oily chemical. The mixture is then injected into branches of the liver artery (hepatic artery) which are supplying the tumour with blood. The oily chemical helps to hold the chemotherapy medicines longer in the liver, and make them more effective in killing cancer cells.
- Radiotherapy.This is a treatment which uses high-energy beams of radiation which are focused on cancerous tissue. This kills cancer cells, or stops cancer cells from multiplying. Radiotherapy is not often used for primary liver cancers apart
form the uncommon cholangiocarcinoma type of cancer.
What is the prognosis?
Overall, the outlook is poor. Many people who develop primary liver cancer are already in poor health with cirrhosis. The best chance of a cure is with surgery when the cancer is small, has not spread from the liver, and the rest of your liver is relatively healthy. However, this situation only occurs in a minority of cases. The various other treatments described above may delay the progression of the disease, but are not often curative.
HOSPITAL ADDRESS
132ft. Ring Road, Helmet Circle, Memnagar, Ahmedabad – 380052. Gujarat, India.
EMERGENCY( 24X7 )
Mobile: +91 – 99047 44410
Help Line : +91 – 98244 40044
+91 – 79 – 2791 4444
E-MAIL ADDRESS
contact@xdemo.app
WHY KAIZEN ?
With a vision to extend World Class healthcare solutions to the community through advances in medical technology, medical research and by adopting best man power management practices , Kaizen hospital was established in Ahmedabad in 2011.

