Kaizen Advance Endoscopy Center
- Gastroenteroloogy services division specializes in the prevention,diagnosis and treatment of diseases of the liver and digestive tract including the stomach, duodenum, gall bladder, biliary tract, pancreas, small intestine and colon.
- Kaizen Hospital has a full range of latest endoscopic facilities including ERCP and EUS, Upper GI and Lower GI Diagnostic and Therapeutic Endoscopies.
- We are providing round-the-clock services to the Gastro Intestinal emergency medical situations like foreign body ingestion, hematemesis, hepatic encephalopathy to name a few.
Endoscopy at Kaizen Hospital
Kaizen Hospital is a state-of-the-art facility equipped with the latest technology and staffed by experienced gastroenterologists, surgeons and endoscopy nurses.
DIAGNOSTIC AND THERAPEUTIC PROCEDURES
Medical Uses
- Confirmation of a diagnosis, most commonly by performing a biopsy of the digestive system to check for conditions such as gastritis, anemia, H. Pylori infection, bleeding, inflammation, cancers and diarrhea.
- Investigation of symptoms in the GI digestive system including nausea, vomiting, abdominal pain, difficulty in swallowing and gastrointestinal bleeding.
Advanced Endoscopic System
- Colonoscopy
- Esophageal Stenting
- Diagnostic EUS
- ERCP to evaluate Bile Duct and Pancreatic Ducts
- Gold Proe Therapy for GI bleeding
- Endoscopic Foreign Body Removal
- Endoscopic Balloon Dilatation
- Pouchoscopy
- PEG
- Sigmoidoscopy
- EUS Guided Therapeutic Procedure
Endoscopy
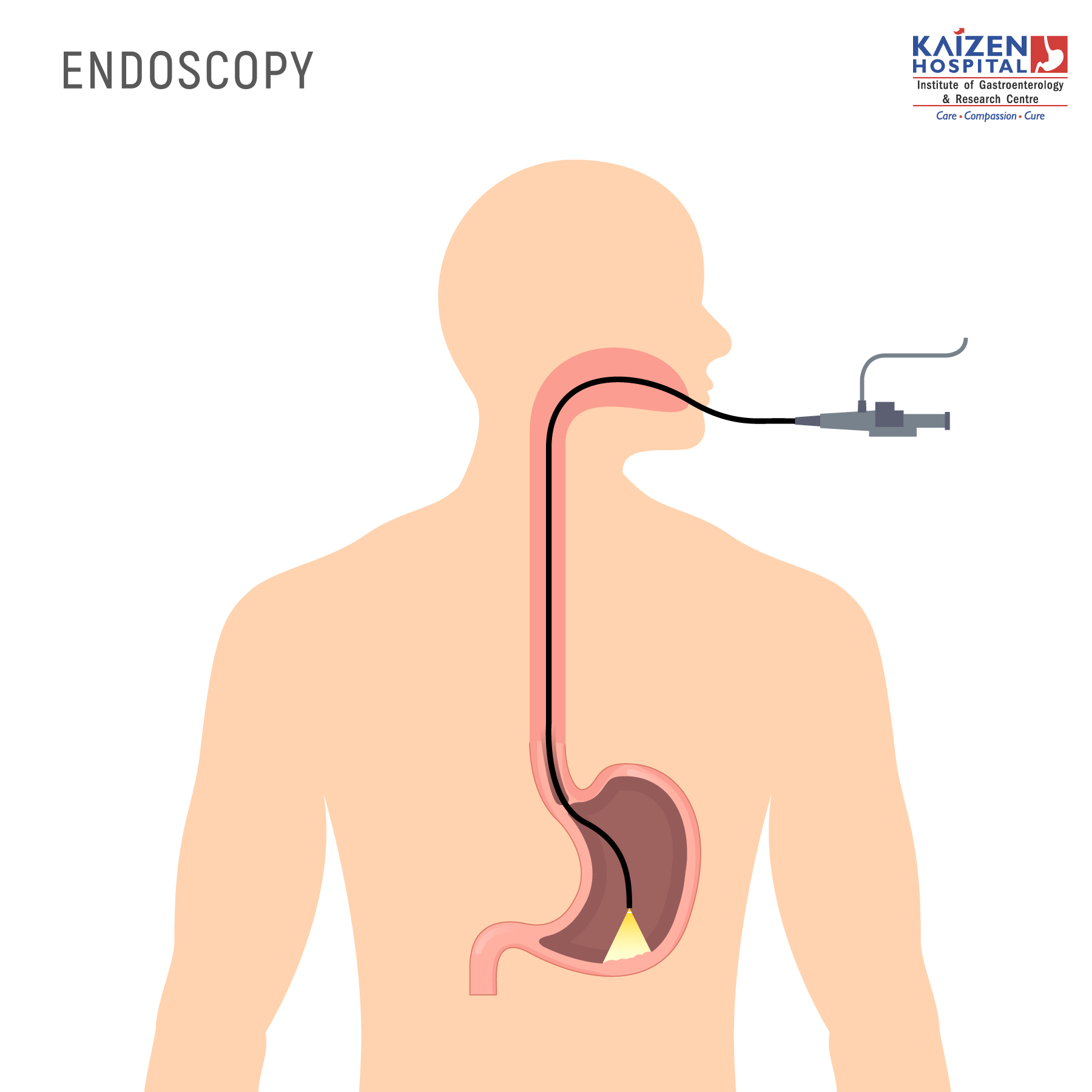
Endoscopy is a procedure that uses specialized tools to visualize and operate on the internal organs of the body. Endoscopy is a minimally invasive diagnostic medical procedure. This procedure allows visualizing the problems within the body without need of making large incisions. An endoscope is used to perform this procedure. An endoscope is a device consisting of a long, thin, flexible tube which has a light and a video camera. With the help of this endoscope image of the inside of the patient’s body can be seen on a monitor screen. The endoscope can also be used for enabling biopsies and retrieving foreign objects. It is a non invasive alternative to surgery for foreign object removal from the gastrointestinal tract. The whole procedure is recorded so that doctor can review it again.
Upper Endoscopy:
This procedure is used to examine upper gastrointestinal tract. An endoscope is easily passed through the mouth and throat and in to the esophagus allowing the doctor to view the esophagus, stomach, and upper part of the small intestine.
Applications of Endoscopy:
Endoscopy is often used to confirm a diagnosis when other devices such as MRI, x ray or CT scan are considered inappropriate.
Most common conditions that can be diagnosed with an endoscopy are:
- Internal bleeding
- Irritable bowel syndrome
- Stomach ulcers
- Chronic diarrhea
- Incontinence
- Cancerous changes in GI lining
Endoscopy is commonly used for the diagnosis of cancer. Samples of tissue to find out whether it is cancerous can be taken using endoscope. Endoscopy is the most effective screening option for colorectal cancer.
Some surgical procedure can be carried out with a modified endoscope, such as the removal of the gall bladder, tying and sealing of the fallopian tubes and taking out small tumors and foreign objects from the lungs or digestive system.
Risks of Endoscopy:
Compared to open surgery, endoscopy has a much lower risk of bleeding and infection. There are some rare complications such as:
- Damage to organs
- Redness
- Swelling
- Fluid or pus discharge
- Pain
- Temperature (fever)
- Piercing or tearing of an organ
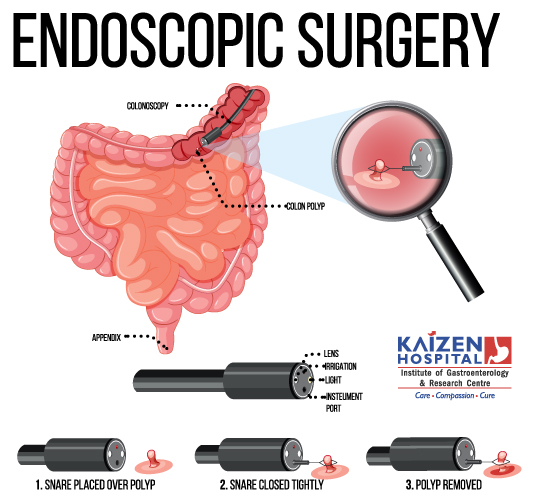
Endoscopic procedure:
Examining the upper gastrointestinal tract requires nothing more than fasting for 6-8 hours prior to the procedure where as to examine the colon, it must be cleared of stool. Therefore a laxative or group of laxatives is given on the day before the procedure.
For most endoscopic procedures a sedative is used. This increases the comfort of the individual undergoing the procedure. The sedative is administered via an injection in to the vein that produces relaxation and light sleep. General anesthesia is given in only very special circumstances.
Colonoscopy
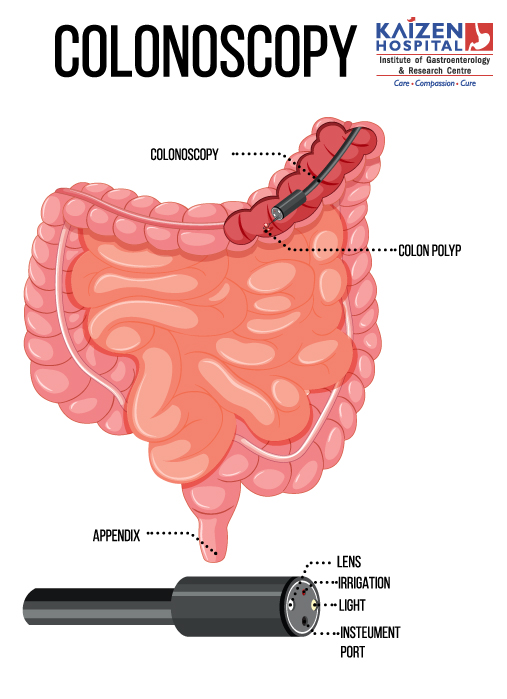
- Minimally invasive test to detect changes or abnormalities in the large intestine (colon) and rectum.
- Polyps or other types of abnormal tissue can be removed through the scope during a colonoscopy.
- Tissue samples (biopsies) can be taken during a colonoscopy.
Indications
- Causes of abdominal pain, rectal bleeding, chronic constipation, chronic diarrhoea and other intestinal problems can be detected.
- Ulcers, colon polyps, tumours, and areas of inflammation or bleeding can be detected.
Preparation
- Nothing to take by mouth on the day of colonoscopy.
- Bowel clearance by laxativeseither the night before colonoscopy, or in the morning of the procedure.
- Avoid taking medicines for Diabetes or any blood thinner agents on the day of procedure.
- During a colonoscopy, patient is sedated to minimize discomfort.
- Patient lies in his side on the examination table, with knees drawn towards chest.
- Long, thin, flexible tube called a colonoscope, which contains a light by which air is pumped into colon, is inserted into the rectum to look at the colon.
- The colonoscope also contains a tiny video camera at its tip which sends images of inside of the colon to an external monitor.
- A colonoscopy usually takes about 20 minutes to an hour.
After the procedure
- After the procedure, it takes about an hour to begin to recover from the sedative.
- Someone may be needed to take the patient home because it can take up to a day for the full effects of the sedative to wear off.
- Patient can’t drive or go back to work for the rest of the day.
- Patient may feel bloated or pass gas for a few hours after the exam, due to passage of air from colon. Walking may help relieve any discomfort.
- Patient may also notice a small amount of blood(rare) with his first bowel movement after the exam.
- Consult doctor in case of persistent bleeding, abdominal pain or a fever.
EUS
- Minimal invasive procedure in which endoscopy is combined with ultrasound to obtain images of the chest and digestive tract, adjacent organs and lymph nodes.
- EUS is performed on an OPD basis and is well-tolerated by most people
Procedure:
- EUS is performed with the patient sedated.
- The endoscope is passed through the mouth and advanced through the esophagus to the suspicious area.
- From various positions between the esophagus and duodenum, organs within and outside the gastrointestinal tract can be imaged to see if they are abnormal, and they can be biopsied by a process called fine needle aspiration (FNA) by inserting a needle through the stomach lining into the target. EUS with FNA lasts about for an hour.
- Organs such as the liver, pancreas, and adrenal glands are easily biopsied, as are any abnormal lymph nodes.
- Gastrointestinal wall can be imaged if it is abnormally thick, suggesting inflammation or malignancy.
- EUS can be used to locate gall stones which may have migrated into the common bile duct.
Advantages of EUS:
- EUS is used to find the cause of symptoms such as abdominal or chest pain, to determine the extent of diseases in digestive tract and lungs.
- EUS may help in the detection of:
- Cancer of the esophagus, lung, stomach, pancreas, colon, ampullary and rectal cancers.
- Lymphoma
- Barrett’s esophagus
- Neuro endocrine tumors
- Pancreatitis and pancreatic cysts
- Bile duct stones
- Rectal fistulas and faecal incontinence
- To assess the depth of the tumour.
- Determine the extent (stage) of cancer.
- Determine if cancer has spread (metastasized) to your lymph nodes or other organs
- Guide drainage of pseudocysts and other abnormal collections of fluid in the abdomen.
- Evaluate abnormal findings from imaging tests, such as cysts of the pancreas.
- Permit precise targeting for delivering medication directly into the pancreas, liver and other organs
Risks:
- Bleeding in case of FNA.
- Pancreatitis, if fine-needle aspiration of the pancreas is done. Infection
- Perforation of intestinal wall.
- larming signs after EUS-
- Fever
- Vomiting
- Difficulty swallowing
- Severe or persistent abdominal pain
- Chest pain
- Shortness of breath
- Black or very dark-coloured stool
Preparation before EUS:
- Nil by mouth before EUS.
- If EUS is being done in rectal area, bowel clearance by laxatives or enema.
- Stop certain medications, such as blood thinners as it may increase risk of bleeding in case of FNA. If you have chronic conditions, such as diabetes or high blood pressure, your doctor will give you specific instructions regarding your medications.
- Arrange for someone to drive you home after the procedure.
ERCP
Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure that combines upper gastrointestinal (GI) endoscopy and x-rays (Fluroscopy) to treat problems of the bile and pancreatic ducts.
What are the bile and pancreatic ducts?
Bile ducts carry bile from your liver to gall bladder and duodenum. Pancreatic ducts carry pancreatic juice from pancreas to duodenum. Small pancreatic ducts empty into the main pancreatic duct. Common bile ducts and main pancreatic duct join before emptying into duodenum.
Indications of ERCP-
- Choledocholithiasis
- Cholangitis
- Acute biliary pancreatitis
- Chronic pancreatitis
- Pancreatic pseudocysts
- Cancer of the bile ducts
- Cancer of the pancreas
How do doctors perform ERCP?
Procedure:
ERCP is performed with the patient sedated.
Duodenoscope passed upto second part of duodenum and locates ampulla.
Sphincteotomy
Cholangiography with contrast medium through the catheter to make the ducts more visible on fluoroscopy
- Dilatation of ducts
- Break up or remove stones
- Brush cytology
- Insert stent
The procedure most often takes between 1 and 2 hours.
What are the risks of ERCP?
- Pancreatitis
- Cholangitis
- Hemorrhage
- Respiratory or cardiac problems
- Perforation of duodenum
Research has found that these complications occur in about 5 to 10 percent of ERCP procedures.
Manometry & pH Metry

- Esophageal Manometry is a computerised instrument to know about the smooth functioning of food pipe in our body.
- The use of 24 hours pH metry is to diagnose the disease of acid reflux
- Anorectal Manometry with biofeedback is a system which trains patient to pass stool by controlling the muscles.
When to use Esophageal Manometry & pH metry?
- Difficulty in swallowing the food(dysphagia)
- When the patient have symptoms like heaviness in chest while swallowing the food
- Burning in throat and chest (heartburn)
When to use Anorectal Manometry?
- Faecal incontinence – when patient passes stool involuntarily
- Increase frequency of stool
- Straining while passing stool
Which kind of diseases can be diagnosed?
- Achalasia Cardia
- Gerd
- Esophageal Scleroderma
- Neurogenic diseases
- Hiatus Hernia
- Esophageal Motility Disorder
- EGJ Outflow Obstruction
- Acid Reflux disease
HOSPITAL ADDRESS
132ft. Ring Road, Helmet Circle, Memnagar, Ahmedabad – 380052. Gujarat, India.
EMERGENCY( 24X7 )
Mobile: +91 – 99047 44410
Help Line : +91 – 98244 40044
+91 – 79 – 2791 4444
E-MAIL ADDRESS
contact@xdemo.app
WHY KAIZEN ?
With a vision to extend World Class healthcare solutions to the community through advances in medical technology, medical research and by adopting best man power management practices , Kaizen hospital was established in Ahmedabad in 2011.

